NECK PAIN DUE TO UNDETECTED METASTATIC LUNG ADENOCARCINOMA
Llumiguano, Carlos*^, Arregui, Elena**^, Borrás, José Maria*^, Villa, José Carlos***^, Gonzalez, Lucia****^
*Neurosurgery Department
**Radiation Oncology Department
*** Medical Oncology Department
**** Pathological Anatomy Department
^Neuro-oncology Committee
University General Hospital of Ciudad Real, Spain
CORRESPONDING AUTHOR:
Dr. Llumiguano, Carlos M.D., Ph.D.
Neurosurgery Department
Universitiy General Hospital of Ciudad Real
C/l Obispo Rafael Torrija
13005 Ciudad Real – Spain
e-mail: carlos.llumiguano@yahoo.com
Abstract
Background context
Computed tomography (CT) and magnetic resonance imaging(MRI) have contributedgreatly tothe ability to identifymetastasesinhead and neckcancer. However the deficienciesin the assessment oflymphadenopathystill exist. On the other hand, in cancer disease the subcutaneous tissue involvement by metastasis is a rare phenomenon, especially the lungcarcinomadoes inabout 0,7 – 9 %.
Purpose
The aim ofthis casereportisto emphasize theimportance ofadequate knowledge ofthepatient’smedical history, physical examination and a detailed analysis of imaging studies.
Study design
Observational case report.
Methods
A 62-year-old man in whom the first manifestation of a metastatic lung adenocarcinoma was advanced severe and incapacitating neck pain of approximately 4 months of progression attributed to a degenerative disc disease of the cervical spine based in the cervical MRI results. During physical exploration showed no neurological deficit, just a pain in the back of the neck and limitation of the cervical spine motion. After detailed analysis ofcervical MRI images, in which we observe the presence of a small nodule of about 1.5cm–s in the posterior subaponeurotic tissue of the cervical region correlated with the location of the trigger point of pain reported by the patient surgery was recommended to get a sample, and then perform the corresponding histopathological study.
This study was performed in our health center and not needed extra funds for processing, and has no conflict of interest.
Results
After radical excision of the lesion by surgery, the sample was sent for the respective histopathological study. This study refers metastases in soft tissue of lung adenocarcinoma, infiltrating fibroadipose tissue and skeletal muscle. Immunohistochemically was positive for cytokeratin7 (CK7 +), thyroid transcription factor-1 (TTF-1 +) and negative for cytokeratin20 (CK20-). Later, once known the results of histopathological studies the patient under went radio-, and chemotherapy treatment.
Conclusions
Don et al. (1995), in 36 neck dissections from patients with squamous cell cancer found a large number of malignant nodes having diameters of less than 10mm. Since the current radiological criteria for assessing the status of the cervical lymph nodes are based largely on size, the findings indicate the major limitations in the detection capabilities of metastatic disease. For this reason it is important the history, the physical examination and a detailed analysis of imaging studies. Because, of this depends that patients receive an adequate treatment for their condition and needs.
Keywords:
Adenocarcinoma, CT, Metastasis, MRI, Neck pain, Pain.
Abbreviations:
CK Cytokeratine
CT Computed tomography
EMG Electromyography
LINAC Linear accelerator
MRI Magnetic Resonance Imaging
SSEP Somatosensory evoked potentials
STIR Short TI Inversion Recovery
TTF Thyroid transcription factor
Background
Neck pain is a common cause of medical consultation. It is estimated that more than half of the population suffers from neck pain at some time in their life, it affects around 10% of the population each year, about 50% of patients report improvement in less than 4 weeks, and more than 70% asymptomatic at the third month, most do not require radiological studies. About 20% of patients have symptoms that exceed 6 months or are recurrent.
CT and MRI have contributed greatly to the ability to identify metastases in head and neck cancer. However the deficiencies in the assessment of lymphadenopathy still exist. On the other hand, in cancer disease the subcutaneous tissue involvement by metastasis is a rare phenomenon that occurs in approximately 5.3% of patients with cancer disease (1,2,3). Metastases from lung carcinoma is usually located in the brain, bone, liver and adrenal tissues(4), affecting the subcutaneous tissue and skin in 0,7–9 % of patients (1,2,5,6,7,8). However,in men represents the most frequent cause of subcutaneous tissue and skin metastasis (24%), due to the high incidence of this tumor (9). The most common location is in the chest, back and abdomen, due to the tendency to affect areas near the primary tumor (2,3,4).
Case report
A 62-year-old man with a history of lung adenocarcinoma treated with surgery and chemoterapy, referred to neurosurgery outpatient clinic due to severe and incapacitating neck pain of approximately 4 months of progression, which increased with movements, and had been treated with anti-inflammatory and muscle relaxant drugs without relief. Pain intensity had increased to the point of sleep deprivation in the recumbent position. During physical exploration found no neurological deficit. However, it was evident neck pain on palpation, and limitation of rotational, flexion and extension movements of the cervical spine. Cervical MRI revealed the presence of degenerative changes of the cervical spine with a disc-osteophytic complex that mainly involves C.V.-VI., C.VI.-VII. segments, with partial obliteration of anterior subarachnoideal space with adequate physiologic lordosis. Not observed suggestive images of clearly protrusion or herniated disc. Somatosensory evoked potentials (SSEP) indicated involvement of the somatosensory pathway conduction by stimulating both lower limbs, probably inferior to C.5. The electromyogram (EMG) showed no signs of acute or chronic cervical radiculopathy in muscles dependent on the myotomes of C.5.-T.1. bilaterally. It was also observed data compatible with entrapment neuropathy of the left median nerve of mild intensity.
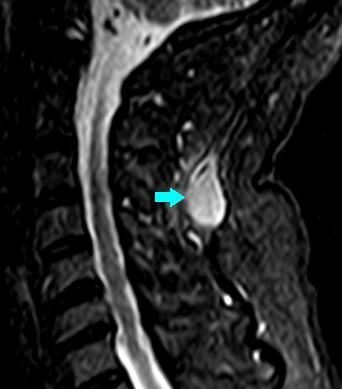
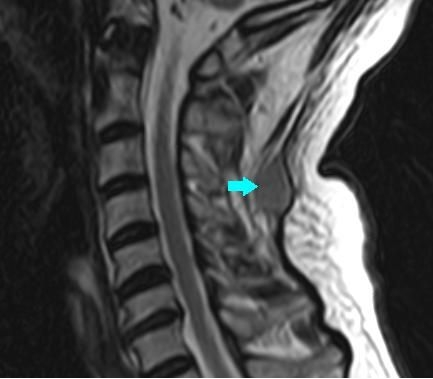
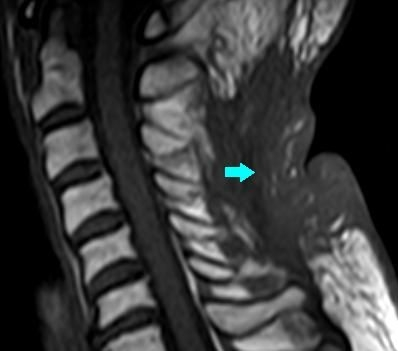
Since the symptoms reported by the patient was not consistent with the physical examination and the results described in the diagnostic studies, we conducted a detailed analysis ofcervical MRI images, in which we observe the presence of a small nodule of about 1.5cm–s hypointense on T1 (Fig. 1), hyperintense on STIR (Fig. 2) in the posterior subaponeurotic tissue of the cervical region correlated with the location of the trigger point of pain reported by the patient. In our view, this nodule more consistent with a malignant lesion was the cause of the patient’s discomfort, so surgery was recommended to get a sample, and then perform the corresponding histopathological study. Prior to surgery, in order to determine the extent of the primary lesion thoracoabdominal CT was requested, the same as compared to previous studies referred disappearance of spiculated nodule located in the left upper lobe and carinal collection of the lung. As a new appearance, was described a characteristic interstitial infiltrate in the right lower lobe and lingular level (pT2aN0 RSL – pT1a LSL). Not showed liver or adrenal lesions.
We performed radical excision of the lesion, and the sample was sent for the respective histopathological study. This study refers metastases in soft tissue of lung adenocarcinoma, infiltrating fibroadipose tissue and skeletal muscle. Immunohistochemically was positive for cytokeratin7 (CK7 +), thyroid transcription factor-1 (TTF-1 +) and negative for cytokeratin20 (CK20-) (Fig. 3). These results were compared witht he previous pathological studies of the primary lung tumor, and they were similar. Based on these studies pathology confirms the diagnosis of metastases in soft tissue of lung adenocarcinoma.
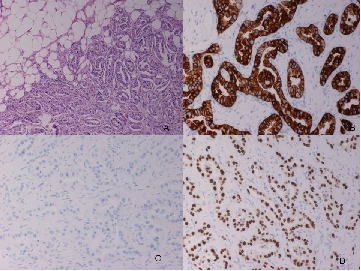
Fig. 3. Images of the histopathological analysis of the nodular lesion with different staining methods. A. Adenocarcinoma infiltrating adipose tissue of neck, HEx10. B. Positive cytoplasmic staining in neoplastic cells for CK7 (CK7x20). C. Negative for CK20 (CK20 x20). D. Nuclear positivity positive with TTF-1 (TTF-1 X20).
Later, once known the results of histopathological studies the patient under went radiotherapy, for which we performed a simulation CT in supine position using a isocentric technique and supported by mold care, and subject with a short thermoplastic mask. Using alinear accelerator (LINAC) radiation therapy was performed with 6 MeV photons to the following volumes:PTV1 – bedding of subaponeurotic lesion. The total dose delivered was 30 Gy, with a fractionation of 300c Gy/ session. The doses toorgans at riskmet the criteria established by QUANTEC tables. Not presented any toxicity. Once completed radiation therapy the patient was referred to outpatient clinic of medical oncology,where continued treatment with carbo – pemetrexed.
After surgery, radiation-, and chemotherapy control cervical MRI was performed at 3, 6, 12, 24 months, which indicate total resection of the lesion with no evidence ofl ocal recurrence (Fig. 4). Currently the patient is stable, and asymptomatic.
Discussion
Don et al. (1995), in 36 neck dissections from patients with squamous cell cancer found a large number of malignant nodes having diameters of less than 10 mm. Since the current radiological criteria for assessing the status of the cervical lymph nodes are based largely on size, the findings indicate the major limitations in the detection capabilities of metastatic disease (10). Therefore it is important to emphasize that, although CT and MRI have contributed greatly to the ability to identify metastases in head and neck cancer, the deficiencies in the assessment of lymphadenopathy still exist. Although we must indicate that in cancer disease the subcutaneous tissue involvement by metastasis is a rare phenomenon, especially the lung carcinoma does in about 0,7–9% (1,2). Based on medical literature, it is important to include the metastatic disease in the differential diagnosis of cervical pain, especially in patients with a history of cancer disease (3), as it can cause symptoms similar to cervical degenerative pathology.
Histologically, the majority of metastases are non-microcitic carcinoma, and especially adenocarcinoma (CK7 +, TTF-1 +, napsin-A + and CK20-) (11,12), as in our case. Generally, subcutaneous tissue and skin metastases are accompanied by metastasis to other levels (9) and are associated with a median survival prognosis of no more than 4 months (4,13).
For this reason it is important the history, the physical examination and a detailed analysis of imaging studies. Because, of this depends that patients receive an adequate treatment fort heir condition and needs.
Bibliography
Krathen RA, Orengo IF, Rosen T. Cutaneous metastasis: a meta-analysis of data. South Med J. 2003;96:164–7.
Perisano C, Spinelli MS, Graci C, Scaramuzzo L, Marzetti E, Barone C, Fabbriciani C, Maccauro G. Soft tissue metastases in lung cancer: a review of the literature. Eur Rev Med Pharmacol Sci. 2012 Dec;16(14):1908-14.
Plaza JA, Perez-Montiel D, Mayerson J, Morrison C, Suster S. Metastases to Soft Tissue. A Review of 118 Cases Over a 30-Year Period. Cancer 2008;112:193–203.
Dhambri S, Zendah I, Ayadi-Kaddour A, Adouni O, El Mezni F. Cutaneous metastasis of lung carcinoma: a retrospective study of 12 cases. J Eur Acad Dermatol Venereol. 2011;25:722–6.
Blanco Villalba JC, Santos R, Batagelj E, Lehmann O, Medina L, Blanco Villalba M, Vega P. Experiencia en el tratamiento del Cáncer de Pulmón. Revisión epidemiológica de los datos clínicos y patológicos. Rev Argent Canc 2004; 32(1):32-40.
Bunn P. Cáncer de pulmón: nuevas combinaciones en el tratamiento del cáncer avanzado de células pequeńas y no pequeńas. Rev Argent Canc 1996; 24(2): 82-7.
Perisano C, Spinelli MS, Graci C, et als. Soft tissue metastases in lung cancer: a review of the literature. Eur Rev Med Pharmacol Sci. 2012 Dec;16(14):1908-14.
Armengot Carbo M, et al. Cervicalgia aguda y nodulo cutaneo como primera manifestacion de un adenocarcinoma pulmonar (Acute cervical pain and cutaneous nodule as the first manifestation of lung adenocarcinoma). Piel (Barc). 2012. doi:10.1016/j.piel.2012.02.008.
Mollet TW, Garcia CA, Koester G. Skin metastases from lung cancer. Dermatol Online J. 2009;15:1.
Don DM, Calcaterra ThC, Anzai Y, Lufkin RB, Fu Y.: Evaluation of cervical lymph node metastases in squamous cell carcinoma of the head and neck.. The Laryngoscope Volume 105, July 1995, Issue 7, pages 669–674.
Stoll LM, Johnson MW, Gabrielson E, Askin F, Clark DP, Li QK. The utility of napsin-A in the identification of primary and metastatic lung adenocarcinoma among cytologically poorly differentiated carcinomas. Cancer Cytopathol. 2010;118:441–9.
Hussein MR. Skin metastasis: a pathologist’s perspective. J Cutan Pathol. 2010;37:e1–20.
Perng DW, Chen CH, Lee YC, Perng RP. Cutaneous metastasis of lung cancer: an ominous prognostic sign. Zhonghua Yi Xue Za Zhi (Taipei). 1996;57:343–7.













Palabras Clave: Adenocarcinoma, CT, Metastasis, MRI, Neck pain, Pain